What is it?
Rheumatoid arthritis is an inflammatory form of arthritis. This disease causes chronic inflammation of the joints and can lead to deterioration of a variety of systems in the body. Rheumatoid arthritis occurs when the immune system attacks the lining of the membrane around the joints known as the synovium, which causes inflammation that thickens the synovium and ultimately deforms the cartilage and bone of the joints.
How common is it and who is at risk?
An estimated one percent of the entire world population suffers from rheumatoid arthritis. As the case with osteoarthritis, women are more likely to develop rheumatoid arthritis. Other groups at risk are people middle-aged or older as well as those suffering from obesity. Rheumatoid arthritis risk is inheritable, which may be accelerated by smoking or unknown environmental exposures.
What are the symptoms?
Signs of the disease include swollen, tender joints that may feel stiff, particularly in the mornings. Fever, fatigue, and loss of activity are also common symptoms. Rheumatoid arthritis tends to manifest initially in the smaller joints like those in the fingers and toes. Symptoms are exhibited in joints of other body parts as the disease spreads.
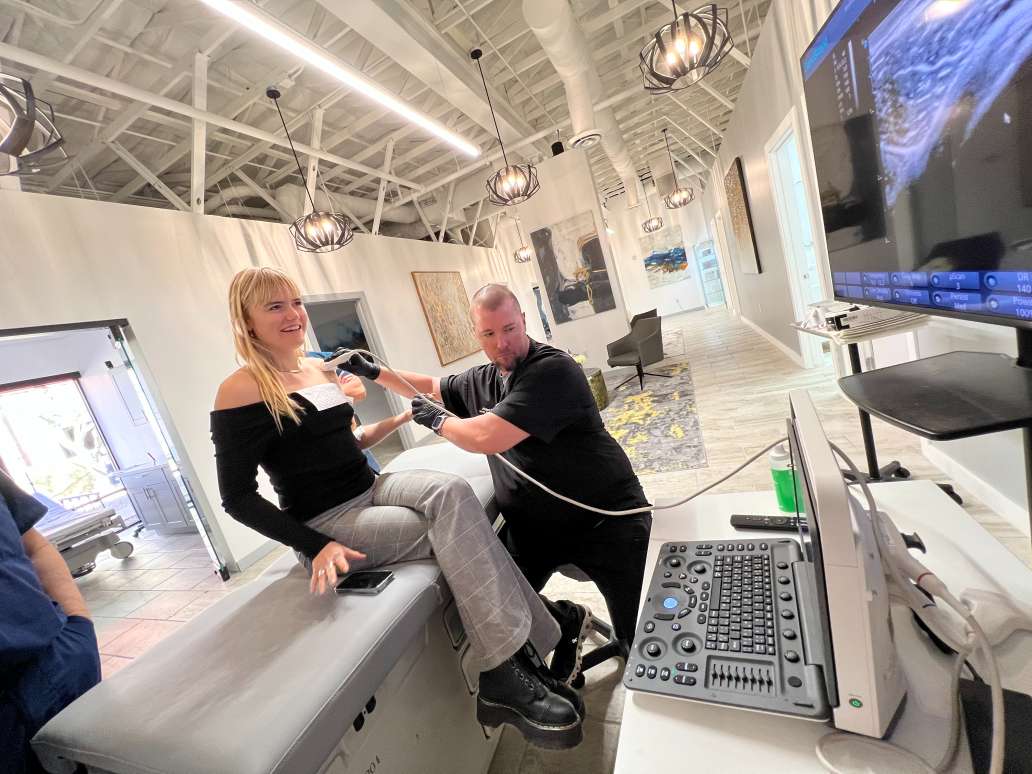
How is it diagnosed?
Diagnosis begins with a physical test checking for redness, warmth, and swelling as well as the state of reflexes in the affected joints. Multiple blood tests are conducted as people with rheumatoid arthritis usually have elevated erythrocyte sedimentation rates and C-reactive protein levels. Additionally, X-rays, MRIs, and ultrasounds are conducted to track the spread of the disease.
What are the treatment options available?
While no cure exists as of now, research has revealed that the symptoms may be controlled by early application of disease modifying anti-rheumatic drugs (DMARDs). Steroids or nonsteroidal anti-inflammatory drugs may be prescribed depending on the case. Exercises to retain joint flexibility also provide some relief. If medications fail to slow down the disease, doctors may recommend surgery to repair or replace joints or swollen tendons.