Call to Schedule Free Consultation at Over 80 Centers Worldwide!
- Home
- Success Stories
- About
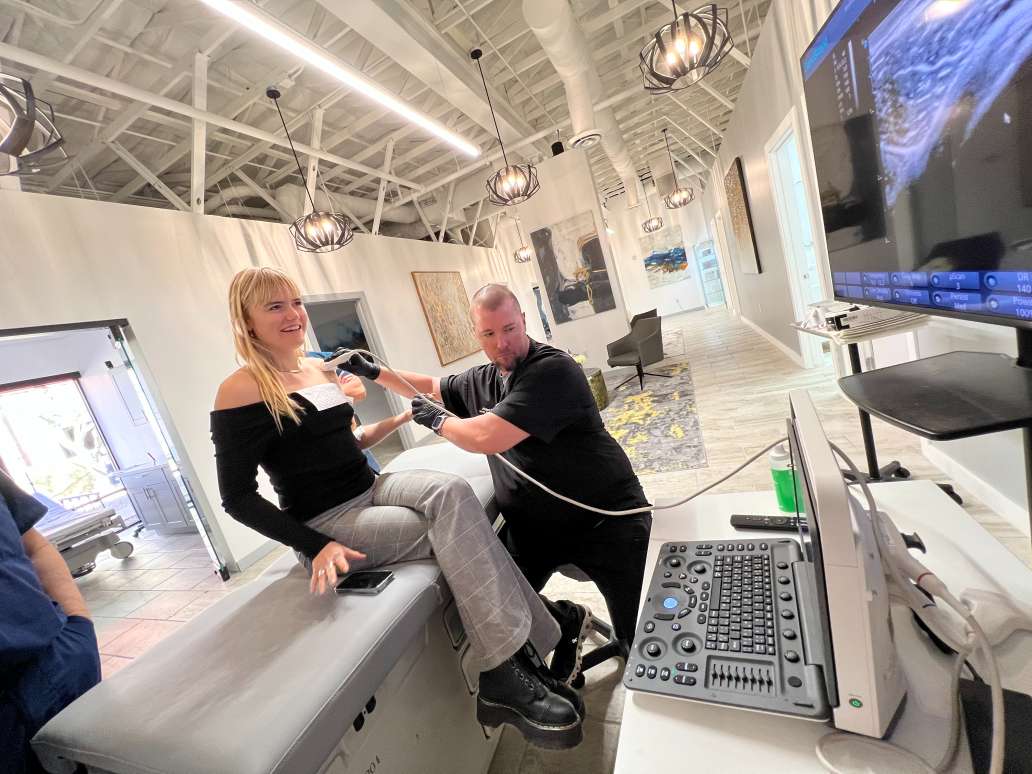
- Stem Cells
- Conditions
Autoimmune
Cardiovascular
Endocrine
Gastrointestinal
Liver
Musculoskeletal
Neurological
Other
Respiratory/Pulmonary
Reproductive
Renal/Kidney
Urologic
- Videos
- Locations
- Home
- Success Stories
- About
- Stem Cells
- Conditions
Autoimmune
Cardiovascular
Endocrine
Gastrointestinal
Liver
Musculoskeletal
Neurological
Other
Respiratory/Pulmonary
Reproductive
Renal/Kidney
Urologic
- Videos
- Locations