A doctor will generally make their diagnosis for trigeminal neuralgia by carrying out a physical examination, reviewing medical history, and conducting specific diagnostic tests. These are carried out to check if the trigeminal nerve is involved and to look for underlying causes of the condition. This is because many other conditions have symptoms similar to trigeminal neuralgia, therefore the need for accurate diagnosis.
Physical examination is based on the description of the pain provided by the patient. These descriptions are classified according to the type of pain (pain associated with trigeminal neuralgia is sudden, electric shock-like, and transient), location (areas of the face affected will indicate the involvement of the trigeminal nerve) and triggers (stimulation of the cheeks by chewing, talking, or even encountering a cool breeze will usually trigger trigeminal neuralgia- related pain).
Medical history review of the patient is also important as it provides vital information other than the symptoms of the condition, enabling a doctor to identify other possible conditions or factors that may be causing pain. This information includes current medications, previous diagnosis, and/or past treatments.
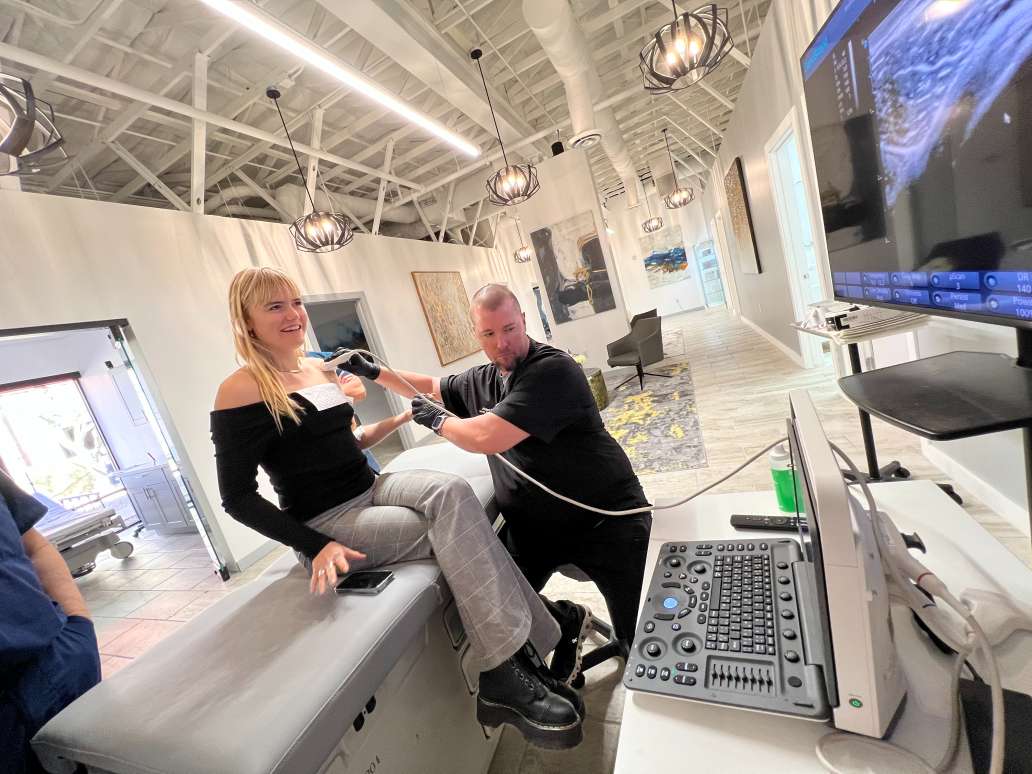
Specific diagnostic tests carried out may be neurological tests or advanced diagnostic tests. An example of a neurological test for diagnosing trigeminal neuralgia is trigeminal reflex testing and this is carried out to examine the facial sensitivity using certain materials and to analyze the sensory responses. Reflex tests like this can help a doctor determine whether the symptoms are caused by a compressed nerve or another condition.
The common types of advanced diagnostic tests for diagnosing trigeminal neuralgia include medical imaging tests, such as Magnetic resonance angiography (MRA) and Magnetic resonance imaging (MRI).
Magnetic resonance angiography is a method used to diagnose trigeminal neuralgia caused by blood vessel compression. This method employs the use of a dye injected into the blood vessel to highlight the blood flow. This method clearly defines the presence and severity of compressions caused by blood vessels on nerves, consequently making it a very effective way for diagnosing trigeminal neuralgia.
Magnetic resonance imaging provides a clear picture of soft tissues, such as the brain, spinal cord, and nerves. This makes it possible to assess nerve integrity and to determine whether trigeminal neuralgia is as a result of multiple sclerosis or tumors.
Advanced diagnostic methods may prove abortive in determining the cause of idiopathic trigeminal neuralgia.
There are a number of other conditions that can mimic the symptoms of trigeminal neuralgia. So, differential diagnosis is necessary in order to be able to accurately diagnose the condition. Some of these conditions are nerve pains such as glossopharyngeal neuralgia, occipital neuralgia. Inflammatory conditions such as dental pain, giant cell arteritis, middle ear infections and sinus infections can also produce similar symptoms as trigeminal neuralgia.
It is very important for the doctor to get an accurate diagnosis as it will ensure that a suitable treatment plan is developed for pain relief.