There is no cure for complex regional pain syndrome, as of now, but a combination of different treatments together can significantly help in controlling the symptoms. Treatments are most effective if started within the first few months when symptoms begin showing up. Treatment combinations are devised on a case to case basis, depending on the type of symptoms and their severity.
Various medications are available to manage symptoms of CRPS. For the mildest cases, over the counter pain relief medicines like ibuprofen could suffice in treating the pain. Opioids might be prescribed for more severe cases for a limited time under proper supervision by the physician. Some antidepressants can ease neuropathic pain. For some individuals, corticosteroids may be prescribed for a time to reduce inflammation in the limb. Other medications include bone-loss medication and sympathetic nerve-blocking medication. Some studies have also come out in favor of intravenous ketamine for pain relief.
Doctors may recommend different types of therapies to cope with the pain and other symptoms. Application of heat or some topical treatments like lidocaine cream can relieve pain, swelling, and hypersensitivity. Mirror therapy is used to trick the brain into improving the functions of the affected limb. The patient is made to sit before a mirror and move the healthy limb, which the brain perceives as the movement of the injured limb.
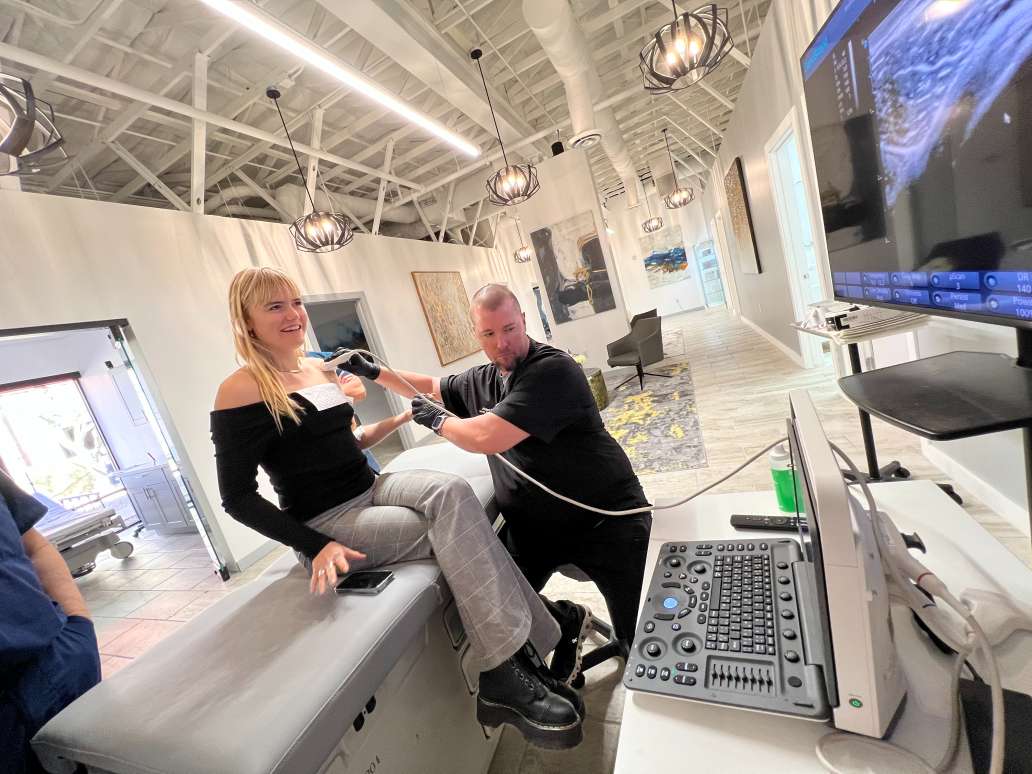
Physical therapy is an important treatment for CRPS. A physical therapist guides the patient through exercising the affected limb to relieve pain, improve range of motion, increase flexibility, endurance, and overall strength. Physical therapy produces much better results if the diagnosis is made in the earlier months of the disease developing.
Other types of therapies are transcutaneous electrical nerve stimulations to reduce pain by applying electrical pulses to the nerve endings, and spinal cord stimulation to ease pain by passing current to the spine. Intrathecal drug pumps involve pumping pain relief medications directly into the spinal fluid. Biofeedback is also an effective form of therapy. Learning biofeedback techniques allow the patient to become more aware and in control of their own body to be able to relieve pain by relaxing their body at will.
Living with a chronic disease can impact a person’s mental health as well. It is not uncommon to go through frequent spells of restlessness, anger, frustration. Ways to minimize the impact are to maintain a daily routine as well as possible, get a healthy amount of rest every night, keep regular contact with friends and family and pursue, as best as one can, passions, interests, and hobbies. If the negative emotions and depressing thoughts remain persistent, it is vital to consult with a doctor or a therapist to get proper, professional help. Regular sessions with a licensed therapist or taking prescribed amounts of antidepressants can vastly improve the patient’s mental health and quality of life.