Amniotic membrane and Wound Care
Introduction
Human amniotic membrane has been use to treat wounds for a long time now. There is resurgence in the use of amniotic membrane to treat wounds due to new techniques that allow for this material to be processed, dried and stored for a long period of time.
The amniotic membrane is a single layer of epithelium that surrounds the developing fetus, separating mother from the fetus. If you examine the membrane under the microscope, you would be able distinguish three layers of collagen, extracellular matrix and regenerative molecules. The extracellular matrix is composed of proteoglycans, laminins, and fibronectin (etc). It consists of type I, III, IV, V and V collagen that add to the structural strength of the membrane.
It also consists of biologically active cells with regenerative properties. These consists of numerous growth factors including fibroblast growth factor (FGF), Platelet derived growth factor (PDGF), metalloproteinase and other such molecules1. Amniotic membrane has a special quality of containing immunosuppressive cytokines that prevent it to be seen as foreign by the mother’s as well as infants immune system2. Amniotic membrane also contains specialized molecules such as defensins that are bactericidal in nature.
What properties make the amniotic membrane suitable to treat wounds?
There are numerous properties of the amniotic membrane that makes it the best fit to treat wounds. The amniotic membrane:
- Increases and hastens the process of wound healing
- Contains numerous cytokines and essential growth factors
- It has bactericidal properties
- Is non-immunogenic
- It reduces pain upon application on a wound
- It provides a ground matrix for the cells to migrate and proliferate
- Reduces inflammation and formation of scar tissue.
What are the Indications for its use?
What types of wounds can be successfully treated with amniotic membrane therapy? Traditionally, amniotic membrane was used to treat burn in the past, but how the practice of using amniotic membrane therapy to treat other types of wounds has increases. This therapy is used only after the conservative treatment has failed as we are most likely to see with chronic and non-healing wounds.

The rates of diabetes are on the rise and the chronic wounds and foot ulcers that are a complication of the disease remain a persistent problem along with chances of amputations for severe cases. To address this problem, numerous medical professionals are now considering human amniotic membrane to treat these wounds. This innovative approach gives the doctors another option to treat wounds that will not heal by using conventional methods. The idea of using this therapy is not new. In 1910; Dr.J.W.Davis at the Johns Hopkins Hospital found that the membrane performed well as a skin graft.
According to the Center for Disease Control and Prevention, diabetic ulcers affect around 15% of people with diabetes, and these wounds lead to around 70,000 amputations annually. Once these ulcers develop, they can be difficult to heal, as bad circulation and nerve damage can persist for years. A study concluded that people 40-70% of the people who underwent amputation surgery do not survive over a period of five years.3
A randomized control trial conducted in 2014 by Charles M.Zelen et all on the use of dehydrated human amniotic membrane allograft for treating diabetic foot ulcers found that 12 out of the 13 people randomly selected to receive this therapy out of the total 25 candidates healed completely over a period of 3 weeks. Out of the 12 patients receiving conservative therapy only 1 recovered. The rest of the 11 started the amniotic membrane graft therapy thereafter and healed completely over the next few weeks. In total 22 out of the 25 patients had healed completely after this therapy.4
Another study on the use of amniotic membrane to treat chronic wounds and ulcer published in 2014 by Gregorio Castellanos et all demonstrated that big chronic wounds with considerable tissue loss, losing the proliferative ability to epithelialize due to inflammatory process can be difficult to treat with conservative therapy. Their study demonstrated that amniotic membrane can induce epithelialization of chronic wounds that are otherwise unable to do so. Amniotic membrane inhibits the anti proliferative effect of transforming growth factor on the keratinocytes, promoting proliferation and migration of cells, allowing the chronic wounds to progress to the state of epithelialization from their non healing state.5
Other studies have also successfully concluded that the use of amniotic membrane therapy to treat superficial burns with exposed nerve endings can lead to fast healing of the wound along with decreasing pain as a result of exposed nerve endings.6
How is the Amniotic membrane applied?
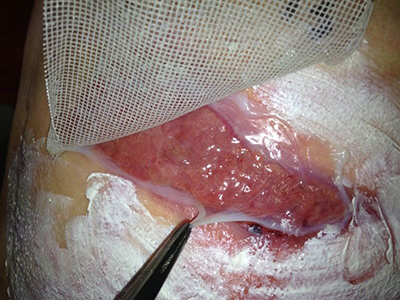
Prior to application of the membrane, a through history of the patient is necessary as to how the wound was formed, any previous treatments and co morbidities. Next the wound bed is prepared b by performing debridement of the wound, removing any necrotic tissue assessing for any signs of infections. Next the membrane is placed on the wound. It would be in cooperated to the wound and significant healing can be seen in terms of size and depth of the wound. A second layer can be applied if slow healing is observed.
Using Amniotic membrane therapy in the management of chronic wounds is a revolutionary and exciting new development which provides an alternative option for wounds that fail to heal after using traditional therapies.
References
- Tseng SC, Espana EM, Kawakita T, Di Pascuale MA, Li W, He H, Liu TS, Cho TH, Gao YY, Yeh LK, Liu CY. How does amniotic membrane work?. The ocular surface. 2004 Jul 1;2(3):177-87.
- Ueta M, KWEON MN, Sano Y, Sotozono C, Yamada J, Koizumi N, Kiyono H, Kinoshita S. Immunosuppressive properties of human amniotic membrane for mixed lymphocyte reaction. Clinical & Experimental Immunology. 2002 Sep 1;129(3):464-70.
- Most RS, Sinnock P. The epidemiology of lower extremity amputations in diabetic individuals. Diabetes care. 1983 Jan 1;6(1):87-91.
- Zelen CM, Serena TE, Fetterolf DE. Dehydrated human amnion/chorion membrane allografts in patients with chronic diabetic foot ulcers: a long-term follow-up study. Wound Medicine. 2014 Feb 28;4:1-4.
- Castellanos G, Bernabé-García Á, Moraleda JM, Nicolás FJ. Amniotic membrane application for the healing of chronic wounds and ulcers. Placenta. 2017 Apr 10.
- Herndon DN, Branski LK. Contemporary Methods Allowing for Safe and Convenient Use of Amniotic Membrane as a Biologic Wound Dressing for Burns. Annals of plastic surgery. 2017 Feb 1;78(2):S9-10.

